Medicines consist of chemical substances. When you ingest a pill, the chemicals in the medicine are absorbed into the bloodstream by the digestive system. From the bloodstream, they pass through the liver and then have an impact on the targeted organ.
Experiencing a headache? Take an Advil and presto! As if by magic, the headache will disappear. Dealing with gas? No need to worry, Tums is available!
The fascinating aspect of modern medicine lies in its ability to solve a wide range of medical issues. However, have you ever pondered how a painkiller like aspirin differentiates between a headache and other types of pain, such as muscle pain? Well, the truth is, it doesn’t possess such knowledge. Despite the impression that these pills specifically target and swiftly alleviate our pain, they are not as sophisticated as we might think. Once ingested, these medications have no direction or awareness of where they need to go within our bodies.
The Journey of Pills in the Body
When we take medicines in the form of tablets, pills, or liquids, they start their journey by being swallowed. From there, they pass through the digestive system, where they are broken down and absorbed into the bloodstream. To reach the liver, they travel through a special pathway known as the hepatic portal vein, which carries the substances from the small intestine to the liver through the bloodstream.
The pill is broken down in the liver and its drug components are released into the bloodstream. Although the drug circulates throughout the body, it does not necessarily have an effect everywhere. Medicines are chemicals that are specifically designed to bind to certain protein molecules in the body, called receptors. Receptors can be found on the surface of cells or inside the cells, and each receptor type has a unique shape, like a lock with a specific key.
When it comes to this situation, the crucial element is the medication. The medication circulates within the body and attaches itself to the lock (receptor) provided that it is a suitable fit.
As an illustration, Advil includes ibuprofen, which acts as a pain reliever. The ibuprofen will attach itself to any pain receptors it encounters as it circulates through the body. Only once it binds to these specific targets can the medication effectively carry out its intended function.
The desired effect is brought about by the ibuprofen entering the cell and initiating chemical reactions. In the case of pain medication, it stops the pain signal from reaching the nerves. For beta-blockers, which are used to control high blood pressure, they attach to the beta receptor located in the cells of the heart, blood vessels, and lungs. By doing so, they prevent adrenaline from binding to the same receptor, stopping it from affecting the cardiac cell and increasing blood pressure. This process is illustrated in the image below. The drug’s ability to bind to its target receptor is essential for all of these actions. However, this natural system is not completely reliable.
Occasionally, medications can attach to receptors that are different from the intended receptor, particularly if their shapes are similar. This is comparable to waving at someone in the distance, believing it’s your friend, but realizing it’s a total stranger when you approach closer.
Regrettably, in this scenario, the wave functions more akin to a greeting, as the medication attaches to the incorrect objective and triggers a sequence of events, leading to undesired repercussions.
What Occurs If Side Effects Arise?
Medications are intended to be consumed in a specific dosage. If taken in lower amounts than the optimal dosage, it may be ineffective in binding to the intended receptor. In such instances, the medication will render entirely futile as it cannot fulfill its intended purpose.
On the other hand, if medications are consumed in larger amounts than the recommended dosage, they have a higher chance of attaching to receptors other than their intended targets. This can lead to unanticipated responses referred to as side effects.
Each drug has a well-known list of typical adverse reactions, such as gastrointestinal discomfort, fatigue, xerostomia, and so on, all of which are indicated on the packaging. Only in extreme situations do these adverse reactions lead to the need for hospitalization.
Therefore, it is crucial to ensure that the correct amount of medication is given in order for it to be effective.
 Image of drug prescription and labelled bottle (Photo Credit: Mr Doomits/Shutterstock)
Image of drug prescription and labelled bottle (Photo Credit: Mr Doomits/Shutterstock)
However, in certain situations, such as with chemotherapy drugs, it is impossible to avoid side effects. Chemotherapy drugs are designed to target cancer cells that grow quickly. Unfortunately, they may also attack other cells that divide rapidly, such as hair cells, resulting in hair loss as a side effect of chemotherapy.
Administering drugs directly to the affected area can reduce the likelihood of side effects. For instance, an antibacterial cream can be applied topically to treat a skin infection. However, this targeted approach is not suitable for all diseases and infections.
Advancements in Medicine with the Use of Smart Drugs
A team of scientists is currently engaged in the development of innovative pharmaceuticals known as ‘smart drugs’. These drugs function similarly to GPS-enabled vehicles, ensuring accurate delivery to the intended destination.
There are cases where drugs can remain inactive near the intended location until they need to be activated. Typically, drugs are eliminated from the body once they detach from the target receptor, requiring regular administration. However, by controlling the activation of drugs, we can maintain a consistent dosage in the body, reducing the need for frequent administration.
In a research study, scientists discovered chemical signals in the body that trigger the release of drugs, leading to the development of an automated drug delivery system. This system delivers the precise dose of medication at the appropriate time, anywhere in the body, with accuracy and effectiveness.
Microchips
Another study investigated the use of microchips implanted under the skin, in the spinal cord, or in the brain to deliver drugs with precision. These microchips contain small reservoirs filled with drugs like chemotherapy or pain medication, which are sealed with gold foil caps. When an electric current of one volt is applied, the caps dissolve, releasing the drug into the body.
Microneedles
Microneedles are a different innovation that uses tiny needles to deliver medication locally. These needles are so small that they do not reach the nerves, making drug delivery painless.
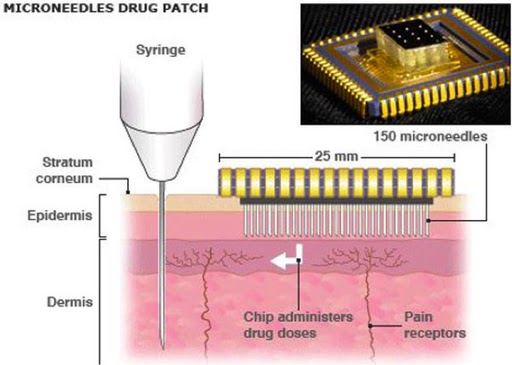
A microneedle drug patch (Photo Credit: National Health FederationWikimedia Commons)
With numerous ongoing studies of this nature, it will not be long before our medications no longer wander aimlessly through our bloodstream. The main question now is whether we can make these “smart” drugs as affordable as the traditional ones!
